Understanding Crohn’s Disease
Understanding Crohn’s Disease: Causes, Symptoms, and Treatment Options
Crohn’s Disease: A Chronic Intestinal Inflammation
Crohn’s disease attacks your digestive tract, causing chronic inflammation. Genetics, environment, and your immune system likely play a role, although the exact cause remains a mystery. It can strike at any age, but most often develops between 15 and 35.
Millions in the US Battle IBD
Inflammatory bowel disease (IBD) extends beyond Crohn’s disease. Shocking data from the Centers for Disease Control and Prevention (CDC) reveals over three million American adults live with either Crohn’s or ulcerative colitis (another form of IBD). This translates to 1.2 million men and 1.9 million women battling IBD in the US, highlighting the significant disease burden.
Genetics and Racial Disparities
Studies reveal a higher prevalence of Crohn’s disease among Ashkenazi Jewish and Caucasian populations, suggesting genetics play a role. The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) states that about 5% to 20% of affected individuals have a close relative with some form of IBD.
Importantly, the study found significant racial disparities in prevalence. Whites have a rate of IBD 7 times higher than Blacks, 6 times higher than Hispanics, and 21 times higher than Asian Americans. More research is needed to understand these racial-ethnic differences in IBD prevalence.
Diagnosing IBD: Uncovering the Culprit
If you experience symptoms suggestive of IBD, your doctor will likely recommend a combination of tests to confirm the diagnosis and identify the specific type of IBD (Crohn’s disease or ulcerative colitis). Here’s a breakdown of some common diagnostic tools:
- Endoscopy/Colonoscopy: These procedures allow doctors to directly visualize the inner lining of your digestive tract for signs of inflammation or ulcers. (Endoscopy for Crohn’s, colonoscopy for ulcerative colitis)
- Imaging Studies: Techniques like contrast radiography, magnetic resonance imaging (MRI), and computed tomography (CT) scans create detailed images of your digestive system. Doctors use these images to assess the extent of inflammation and identify potential complications.
- Stool Sample Analysis: Analyzing your stool helps rule out other conditions and identify the presence of blood or inflammatory markers.
- Blood Tests: Blood tests check for anemia, infection, and inflammation markers to support the IBD diagnosis.
Treating IBD: Taking Control
While there’s no cure for IBD, various treatment options exist to manage symptoms, induce and maintain remission, and improve overall quality of life. Here’s an overview of common treatment approaches:
- Medications:
- 5-aminosalicyclic acids: These medications reduce inflammation in the digestive tract.
- Immunomodulators: These drugs suppress the immune system’s response that can contribute to inflammation.
- Corticosteroids: Effective for reducing inflammation during flares, corticosteroids are typically used for short-term relief due to potential side effects with long-term use.
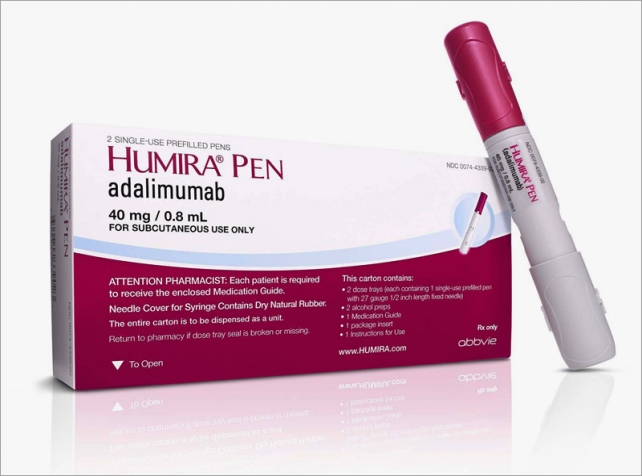
- Biologics: These newer medications target specific components of the immune system involved in inflammation and show promise in managing IBD.
- Surgery: Sometimes surgery may be necessary to remove damaged portions of the gastrointestinal tract, for patients with severe complications. It can be done also for those who don’t respond well to medications.
Finding Relief with Crohn’s
If you have Crohn’s disease, you’re not alone. With proper diagnosis and a personalized treatment plan, you can manage your condition and achieve a good quality of life.
Remember, consulting a healthcare professional is essential to discuss your specific situation and determine the most appropriate course of treatment for you.