Rheumatoid Arthritis: Symptoms and Treatment Options
Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes joint inflammation and pain. It occurs when the immune system mistakenly attacks the synovium, the lining of the joints.
RA predominantly affects the hands, knees, and ankles, usually on both sides of the body. Women are more likely than men to develop RA, and it often occurs in middle age. While the exact cause of RA is unknown, it is believed to be a combination of genetic and environmental factors.
Common symptoms of RA include joint pain, swelling, and morning stiffness lasting for at least six weeks. RA can also affect other parts of the body, such as the eyes, heart, lungs, and blood vessels. Early diagnosis and treatment by a rheumatologist are crucial to managing the disease and preventing joint and organ damage. Treatment goals include reducing inflammation, relieving symptoms, preventing complications, and improving overall well-being. Self-care measures, such as a healthy diet, regular exercise, stress reduction techniques, and support systems, can also play a significant role in managing RA.
Key Takeaways:
- Rheumatoid arthritis is a chronic autoimmune disease that causes joint inflammation and pain.
- Common symptoms include joint pain, swelling, and morning stiffness lasting for at least six weeks.
- Early diagnosis and treatment are crucial for managing the disease and preventing joint and organ damage.
- Treatment goals include reducing inflammation, relieving symptoms, and improving overall well-being.
- Self-care measures, such as a healthy diet, regular exercise, and stress reduction techniques, are important for managing RA.
Causes of Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease that occurs when the immune system mistakenly attacks the body’s own tissues, specifically the synovium in the joints. While the exact cause of RA is not fully understood, it is believed to be a combination of genetic and environmental factors. Certain genes may predispose individuals to develop RA, and external factors such as infections, physical or emotional stress, and other environmental triggers can activate the immune system and lead to the development of the disease. Research is ongoing to further understand the underlying causes of RA and how these factors interact.
It is important to note that rheumatoid arthritis is not caused by a single factor, but rather a complex interplay of genetic and environmental influences. Genetic factors can increase the susceptibility to develop RA, while environmental triggers can initiate the immune response that leads to joint inflammation and damage. Although there is no way to prevent rheumatoid arthritis, knowing the potential causes can help individuals with a family history of RA be aware of their increased risk and take proactive steps to manage their health and well-being.
In summary, the causes of rheumatoid arthritis involve a combination of genetic and environmental factors. While certain genes may increase the risk of developing RA, external triggers such as infections and stress can activate the immune system and lead to the development of the disease. Understanding these causes can help individuals with RA and their healthcare providers better manage the condition and develop targeted treatment plans.
Factors Contributing to Rheumatoid Arthritis
When it comes to the causes of rheumatoid arthritis, there are several factors that play a role in the development and progression of the disease:
- Genetic Factors: Certain genes have been linked to an increased susceptibility to rheumatoid arthritis. Individuals with a family history of RA are more likely to develop the disease.
- Environmental Factors: Infections, physical or emotional stress, and exposure to certain environmental triggers can activate the immune system and initiate the development of RA in genetically susceptible individuals.
- Autoimmune Response: Rheumatoid arthritis is an autoimmune disease, which means that the immune system mistakenly attacks the body’s own tissues, specifically the synovium in the joints. This autoimmune response leads to joint inflammation, damage, and pain.
By understanding the factors contributing to rheumatoid arthritis, individuals and their healthcare providers can work together to manage the condition effectively and minimize its impact on daily life.
| Factors | Description |
|---|---|
| Genetic Factors | Certain genes have been linked to an increased susceptibility to rheumatoid arthritis. |
| Environmental Factors | Infections, physical or emotional stress, and exposure to certain triggers can activate the immune system and initiate the development of RA. |
| Autoimmune Response | Rheumatoid arthritis is an autoimmune disease, where the immune system mistakenly attacks the body’s own tissues, leading to joint inflammation and damage. |
Symptoms of Rheumatoid Arthritis
Rheumatoid arthritis (RA) can manifest with a range of symptoms, each person experiencing a unique combination. However, there are common signs to watch out for. The most prevalent symptom is persistent joint pain, which can be accompanied by tenderness and swelling. This pain is often worse in the mornings and can last for at least six weeks. Additionally, individuals with RA may experience fatigue and a general feeling of being unwell. It is important to note that RA symptoms can come and go, with periods of increased inflammation known as flares.
The disease typically affects multiple joints, and it tends to mirror on both sides of the body. For example, if the right hand is affected, the left hand is likely to experience similar symptoms. Morning stiffness lasting for 30 minutes or longer is another characteristic symptom of RA. This stiffness can make it challenging to perform daily tasks and can improve with gentle movement and activity. It is crucial to pay attention to these symptoms and seek medical evaluation for an accurate diagnosis and appropriate management.
Joint Pain
Joint pain is one of the key symptoms of rheumatoid arthritis. It is often described as a dull ache or a sharp, stabbing sensation. The pain can occur in multiple joints, such as the hands, wrists, knees, and ankles. In some cases, the pain can be severe and debilitating, interfering with daily activities and reducing quality of life.
Joint Swelling
In addition to pain, individuals with rheumatoid arthritis may experience joint swelling. Swelling may cause the affected joints to appear larger or feel warm to the touch. The swelling is a result of inflammation in the synovial membrane, which lines the joints. This inflammation can lead to the accumulation of fluid in the joint, causing it to enlarge and become tender.
Morning Stiffness
Morning stiffness lasting for 30 minutes or longer is a hallmark symptom of rheumatoid arthritis. Individuals with RA may find it challenging to initiate movement in the morning, experiencing stiffness and reduced range of motion in their joints. The stiffness tends to improve with gentle movement and activity throughout the day. It is important to note that morning stiffness can also occur after periods of prolonged inactivity during the day.
Effects of Rheumatoid Arthritis on the Body
Rheumatoid arthritis can have wide-ranging effects on different parts of the body beyond just the joints. The chronic inflammation associated with RA can lead to several complications in various organs and systems. Some of the common effects of rheumatoid arthritis include:
- Eye complications: RA can cause inflammation in the eyes, resulting in dryness, pain, redness, and increased sensitivity to light. Regular eye examinations are crucial to detect and manage these complications.
- Respiratory complications: Inflammation in the lungs can lead to shortness of breath, chest pain, and even lung diseases such as interstitial lung disease. Regular monitoring and appropriate treatment are necessary to maintain lung health.
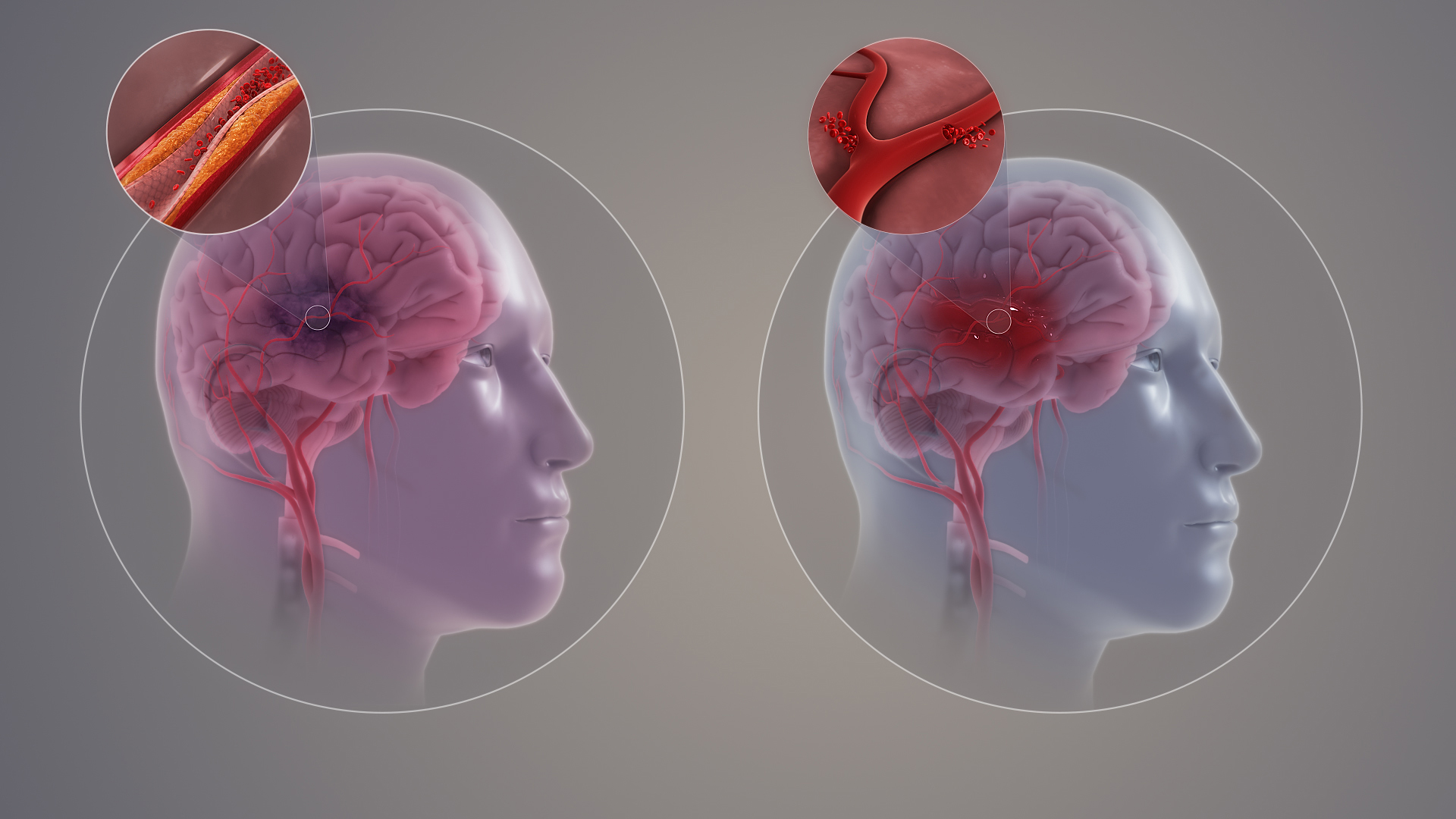
- Heart complications: Rheumatoid arthritis increases the risk of cardiovascular diseases, including heart attack and stroke. The inflammation associated with RA can damage the blood vessels and increase the risk of atherosclerosis. It’s important to manage cardiovascular risk factors, such as high blood pressure and cholesterol, and maintain a healthy lifestyle.
- Joint pain and stiffness: The hallmark of rheumatoid arthritis is joint pain and stiffness. Besides causing discomfort, severe joint pain can limit mobility and impact daily activities.
“The chronic inflammation associated with rheumatoid arthritis can have a significant impact on different organs and systems in the body, leading to complications such as eye problems, respiratory issues, heart conditions, and persistent joint pain.”
It’s essential for individuals with rheumatoid arthritis to work closely with their healthcare team to monitor and manage these effects. Regular check-ups, appropriate treatment, and adopting a comprehensive management plan can help mitigate the impact of these complications on overall health and well-being. It’s also crucial to maintain a healthy lifestyle, including regular exercise, a balanced diet, and stress reduction techniques, to support overall health and improve the management of rheumatoid arthritis.
| Effects of Rheumatoid Arthritis | Common Symptoms/Complications |
|---|---|
| Eye complications | Dryness, pain, inflammation, sensitivity to light |
| Respiratory complications | Shortness of breath, chest pain, lung diseases |
| Heart complications | Cardiovascular diseases, increased risk of heart attack and stroke |
| Joint pain and stiffness | Discomfort, limited mobility, impact on daily activities |
Diagnosis of Rheumatoid Arthritis
When it comes to diagnosing rheumatoid arthritis (RA), it is important to consult with a rheumatologist, a specialist in joint disorders. The diagnostic process typically involves several steps to accurately identify and confirm the presence of RA.
Gathering Medical History
The first step in the diagnosis is a comprehensive review of your medical history. This includes discussing your joint symptoms, their duration, and any family history of autoimmune diseases. Your rheumatologist will ask you questions about the specific joints affected, the nature of your pain, and any other symptoms you may be experiencing. This information helps them assess the likelihood of RA and guide further testing.
Physical Examination
After reviewing your medical history, a physical examination will be conducted. During this examination, your rheumatologist will assess your joints for tenderness, swelling, limited movement, and signs of inflammation. They may also check for the presence of rheumatoid nodules, which are small lumps that can develop under the skin. The physical examination provides important clues to support the diagnosis of RA.
Blood Tests and Imaging
In addition to the medical history and physical examination, blood tests are an essential part of the diagnostic process for RA. Several specific blood markers can indicate the presence of inflammation and help confirm the diagnosis. These markers include erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), rheumatoid factor (RF), and antibodies to cyclic citrullinated peptide (CCP). An elevated level of these markers suggests active inflammation in the body.
Imaging tests, such as X-rays, ultrasounds, or magnetic resonance imaging (MRI) scans, may also be recommended to evaluate joint damage and monitor the progression of the disease. These imaging techniques can provide visual evidence of joint deterioration, swelling, and cartilage damage.
The combination of medical history, physical examination, blood tests, and imaging results allows your rheumatologist to make an accurate diagnosis of rheumatoid arthritis. Early detection and intervention are crucial for effective management of the disease, and prompt diagnosis enables timely treatment to minimize joint and organ damage.
Treatment Options for Rheumatoid Arthritis
When it comes to managing rheumatoid arthritis (RA), there are various treatment options available to help reduce inflammation, relieve symptoms, and protect joints and organs. The goal of treatment is to improve overall well-being and enhance your quality of life. Here are some key treatment options you can discuss with your healthcare team:
HUMIRA could be an option for you. This prescription medicine used alone, with methotrexate, or with certain other medicines to reduce the signs and symptoms of moderate to severe rheumatoid arthritis in adults, may prevent further damage to your bones and joints, and may help your ability to perform daily activities
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), biologics, and corticosteroids are commonly prescribed to manage inflammation and pain. Your doctor will determine the most appropriate medication for your specific needs.
- Lifestyle modifications: Making lifestyle changes can have a significant impact on managing RA. Regular exercise, maintaining a healthy diet, stress reduction techniques, and getting support from a healthcare team and support groups can all play a crucial role in managing the disease.
It’s important to work closely with your healthcare team to develop an individualized treatment plan that addresses your specific needs. They will consider factors such as the severity of your symptoms, your overall health, and any other medical conditions you may have. By following your treatment plan and making proactive choices, you can effectively manage your rheumatoid arthritis and protect your joints and organs.
Table: Comparison of Rheumatoid Arthritis Treatment Options
| Treatment | Description | Benefits |
|---|---|---|
| Medications | Includes NSAIDs, DMARDs, biologics, and corticosteroids | Reduces inflammation, relieves pain, slows down disease progression |
| Lifestyle Modifications | Incorporates regular exercise, healthy diet, stress reduction techniques, and support systems | Improves overall well-being, enhances joint flexibility, and improves quality of life |
| Therapies | May include physical therapy and occupational therapy | Provides targeted exercises and strategies to improve joint function and daily living |
| Surgery | Considered in severe cases to repair or replace damaged joints | Restores joint function and reduces pain |
It’s important to remember that each person’s experience with rheumatoid arthritis is unique, and what works for one person may not work for another. Your healthcare team will work closely with you to develop an individualized treatment plan that suits your specific needs and goals.
By actively participating in your treatment plan and making informed decisions, you can effectively manage your rheumatoid arthritis, reduce inflammation, relieve symptoms, and protect your joints and organs.
Self-Care Strategies for Rheumatoid Arthritis
Effectively managing rheumatoid arthritis involves a holistic approach that goes beyond medical treatment. Implementing self-care strategies in your daily routine can play a significant role in improving your quality of life and managing the symptoms of RA. Here are some self-care practices to consider:
1. Healthy Eating
A well-balanced diet can help support overall wellness and manage inflammation associated with rheumatoid arthritis. Include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats in your meals. Omega-3 fatty acids, found in fatty fish like salmon, can help reduce inflammation. Limiting processed foods, saturated fats, and refined sugars is also beneficial for managing RA.
2. Regular Exercise
Engaging in regular physical activity can improve joint flexibility, strengthen muscles, and reduce pain associated with rheumatoid arthritis. Aim for a mix of aerobic exercises, such as walking or swimming, and strength-training exercises to maintain joint function and overall fitness. Consult with your healthcare provider or a physical therapist to develop an exercise plan tailored to your needs and abilities.
3. Stress Reduction
Stress can worsen symptoms of rheumatoid arthritis. Practice stress reduction techniques, such as deep breathing exercises, meditation, or yoga, to help manage stress levels and promote relaxation. Taking breaks throughout the day, prioritizing self-care activities, and engaging in hobbies or activities that bring you joy can also contribute to your overall well-being.
4. Pain Management Techniques
Explore pain management techniques that work for you. Hot and cold treatments, topical analgesics, or using assistive devices like splints or braces can help alleviate joint pain and stiffness. Additionally, staying on top of your medication regimen prescribed by your healthcare provider can effectively manage pain associated with rheumatoid arthritis.
By incorporating these self-care strategies into your daily routine, you can actively participate in managing your rheumatoid arthritis and improve your overall well-being. Remember to consult with your healthcare provider for personalized advice and guidance tailored to your specific needs.
Supplements and Complementary Therapies for Rheumatoid Arthritis
While medical treatment is essential in managing rheumatoid arthritis (RA), some individuals may find supplements and complementary therapies helpful as adjunct therapies. It’s important to note that these should not replace traditional medical treatment, but they can be used alongside it to enhance symptom management and overall well-being.
One supplement that has shown promise in reducing RA-related pain and morning stiffness is curcumin, a compound found in turmeric. Studies have suggested that curcumin has anti-inflammatory properties and may help alleviate joint symptoms. Omega-3 fish oil supplements have also been studied for their potential benefits in RA. Omega-3 fatty acids have anti-inflammatory effects and may help reduce joint inflammation and pain. However, it’s essential to consult with a healthcare provider before starting any supplements, as they may interact with other medications or have potential side effects.
Complementary therapies such as acupuncture, acupressure, and massage have also been used by some individuals with RA to manage symptoms. These therapies aim to promote relaxation, reduce pain, and improve overall well-being. However, the effectiveness of these therapies can vary from person to person, and it’s important to discuss them with a healthcare professional and seek services from qualified practitioners.
Remember, finding the right combination of treatments for RA is highly individualized, and what works for one person may not work for another. It’s important to work closely with your healthcare team to develop an individualized treatment plan that addresses your specific needs and goals.
| Supplement/Therapy | Potential Benefits | Considerations |
|---|---|---|
| Curcumin (found in turmeric) | – Reduces RA-related pain – Alleviates morning stiffness |
– Consult with healthcare provider before use – Potential interactions with other medications |
| Omega-3 fish oil | – Reduces joint inflammation and pain | – Consult with healthcare provider before use – Potential interactions with other medications |
| Acupuncture, acupressure, and massage | – Promotes relaxation – Reduces pain and stiffness – Improves overall well-being |
– Discuss with healthcare provider – Seek qualified practitioners |
Emotional Well-being and Support for Rheumatoid Arthritis
Living with rheumatoid arthritis can be emotionally challenging. The daily pain, physical limitations, and uncertainty about the future can take a toll on your mental health. However, by focusing on emotional well-being and building a strong support system, you can effectively navigate the emotional impact of living with RA.
A positive attitude plays a significant role in managing rheumatoid arthritis. Maintaining a hopeful outlook, practicing gratitude, and embracing a mindset of resilience can help you cope with the challenges of the disease. It’s crucial to acknowledge your emotions and allow yourself to grieve or feel frustrated at times. Seeking professional help, such as therapy or counseling, can provide a safe space to process these emotions and develop strategies to manage them.
Building a support system is vital for emotional well-being. Surround yourself with friends, family, and understanding healthcare providers who can provide the necessary empathy and encouragement. Online support groups and community organizations can also connect you with others who understand the unique challenges of living with RA. Sharing experiences, advice, and coping strategies can provide a sense of belonging and validation.
“Living with rheumatoid arthritis can be emotionally challenging, but finding emotional support and embracing a positive attitude can make a significant difference in managing the disease and improving your overall well-being.”
Pain management resources are crucial in promoting emotional well-being for individuals with rheumatoid arthritis. Learning and implementing effective pain management techniques, such as relaxation exercises, meditation, and deep breathing, can help alleviate stress and reduce pain levels. It’s important to work with healthcare professionals to develop a comprehensive pain management plan tailored to your specific needs. They can provide valuable guidance and prescribe appropriate pain medications or therapies when necessary.
Emotional well-being plays a vital role in effectively managing rheumatoid arthritis. By cultivating a positive attitude, building a support system, and utilizing pain management resources, you can enhance your overall well-being and successfully navigate the emotional challenges of living with RA.
Conclusion
In conclusion, rheumatoid arthritis is a chronic autoimmune disease that causes joint inflammation and can have various effects on the body. While the exact cause of RA is not fully understood, genetics and environmental factors play a role in its development. Early diagnosis and timely intervention are crucial for effective management of the disease.
Treatment options for rheumatoid arthritis include medications to reduce inflammation, relieve symptoms, and protect joints and organs. However, self-care strategies are also vital in complementing medical treatment. Engaging in healthy eating habits, regular exercise, stress reduction techniques, and utilizing complementary therapies can greatly improve quality of life for individuals with RA.
Additionally, having a strong support system and utilizing resources for pain management and emotional well-being are integral aspects of living with rheumatoid arthritis. By understanding and implementing symptom management strategies, treatment options, and self-care measures, individuals with RA can actively manage the disease and improve their overall well-being.
FAQ
What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes joint inflammation and pain.
What causes rheumatoid arthritis?
The exact cause of RA is not fully understood, but it is believed to be a combination of genetic and environmental factors.
What are the symptoms of rheumatoid arthritis?
Common symptoms of RA include joint pain, swelling, and morning stiffness lasting for at least six weeks.
How does rheumatoid arthritis affect the body?
Rheumatoid arthritis can affect various parts of the body, including the eyes, heart, lungs, and blood vessels.
How is rheumatoid arthritis diagnosed?
A rheumatologist will typically conduct a thorough medical history review, physical examination, and may recommend blood tests and imaging tests for diagnosis.
What are the treatment options for rheumatoid arthritis?
Treatment for RA involves a combination of medications, lifestyle modifications, and self-care measures to reduce inflammation, relieve symptoms, and prevent joint and organ damage.
What self-care strategies can help manage rheumatoid arthritis?
Self-care strategies such as a healthy diet, regular exercise, stress reduction techniques, and pain management techniques can play a significant role in managing RA.
Are there any supplements or complementary therapies that can help with rheumatoid arthritis?
While not a replacement for medical treatment, supplements like curcumin and omega-3 fish oil, as well as complementary therapies like acupuncture and massage, may provide some relief for RA symptoms.
How can I support my emotional well-being while living with rheumatoid arthritis?
Building a strong support system and utilizing resources for pain management and emotional well-being can help individuals cope with the challenges of living with RA.
What is the key takeaway about rheumatoid arthritis?
By understanding the symptoms, treatment options, and implementing self-care measures, individuals with RA can actively manage the disease and improve their overall well-being.
Source Links
- https://www.arthritis.org/diseases/rheumatoid-arthritis
- https://www.niams.nih.gov/health-topics/rheumatoid-arthritis
If you need to take Humira, you may use this coupon to reduce your monthly cost
Don’t Miss It!
Use coupon code 4MG9N2Q7 to get a $150 discount on Humira today!