Preventing Blood Clots; Reducing Stroke Risk with Eliquis
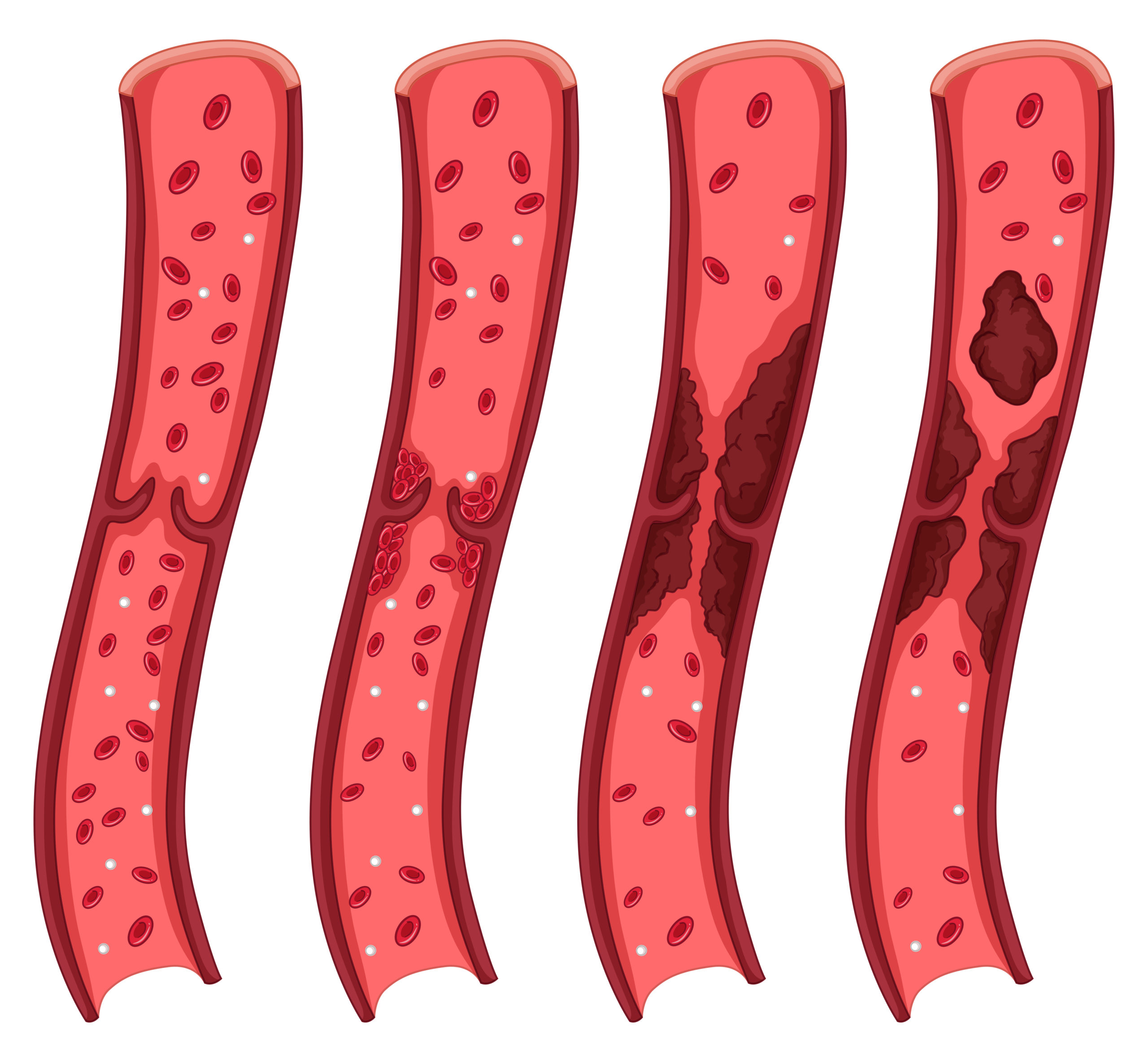
Eliquis is an oral anticoagulant that plays a vital role in preventing blood clots and reducing the risk of stroke, particularly in patients with nonvalvular atrial fibrillation (NVAF). By inhibiting the clotting protein factor Xa, Eliquis effectively reduces the formation of blood clots, helping to maintain a healthy circulation and decrease the chances of stroke or systemic embolism.
Key Takeaways:
- Eliquis is an oral anticoagulant used to prevent blood clots and reduce the risk of stroke in patients with nonvalvular atrial fibrillation.
- Premature discontinuation of Eliquis can increase the risk of thrombotic events, so it should only be stopped for specific medical reasons.
- Regular monitoring for bleeding and adherence to therapy is crucial for patients receiving Eliquis.
- Eliquis carries a risk of bleeding, and patients should be aware of the signs and symptoms of bleeding and seek immediate medical attention if they occur.
- Alongside medical treatment, lifestyle modifications, such as regular exercise and avoiding prolonged periods of immobility, can help prevent blood clots naturally.
The Pharmacology of Eliquis
Eliquis, also known by its generic name apixaban, is a potent and selective factor Xa inhibitor. It directly and selectively inhibits both free and clot-bound factor Xa, reducing the generation of thrombin and subsequently decreasing blood clot formation.
Unlike other anticoagulants, Eliquis does not require the presence of antithrombin III to exert its anticoagulation effect. It is primarily metabolized by the liver and eliminated through both renal and fecal routes.
The recommended dosage of Eliquis varies depending on the indication for use, and it should be taken consistently as prescribed by a healthcare professional.
Thrombin Generation and Anticoagulation Effect
Eliquis effectively reduces thrombin generation by directly inhibiting factor Xa. This interruption stops the cascade leading to thrombin production, a vital part of clotting. This action makes Eliquis a potent anticoagulant, lowering stroke and systemic embolism risks in nonvalvular atrial fibrillation patients. –
| Pharmacokinetic Properties | Information |
|---|---|
| Metabolism | Primarily metabolized by the liver |
| Elimination | Eliminated through renal and fecal routes |
| Dosage | Varies depending on indication, follow healthcare professional’s instructions |
Eliquis has shown significant efficacy in clinical trials, demonstrating its ability to reduce the incidence of stroke and systemic embolism compared to placebo. Its selective inhibition of factor Xa, along with its favorable pharmacokinetic properties, make it a valuable option in the prevention of blood clots and reduction of stroke risk in patients with nonvalvular atrial fibrillation.
Safety Considerations for Eliquis
Using Eliquis requires understanding safety precautions to reduce thrombotic risks and complications. Stopping this anticoagulant early raises thrombotic risk, so follow your healthcare professional’s prescribed regimen.
Switching or stopping Eliquis without adequate anticoagulant coverage can be risky, leading to adverse effects. Patients on Eliquis face potential spinal or epidural hematoma risks with neuraxial anesthesia or spinal puncture, potentially causing long-term paralysis. Thus, weigh risks and benefits of these procedures for Eliquis users.
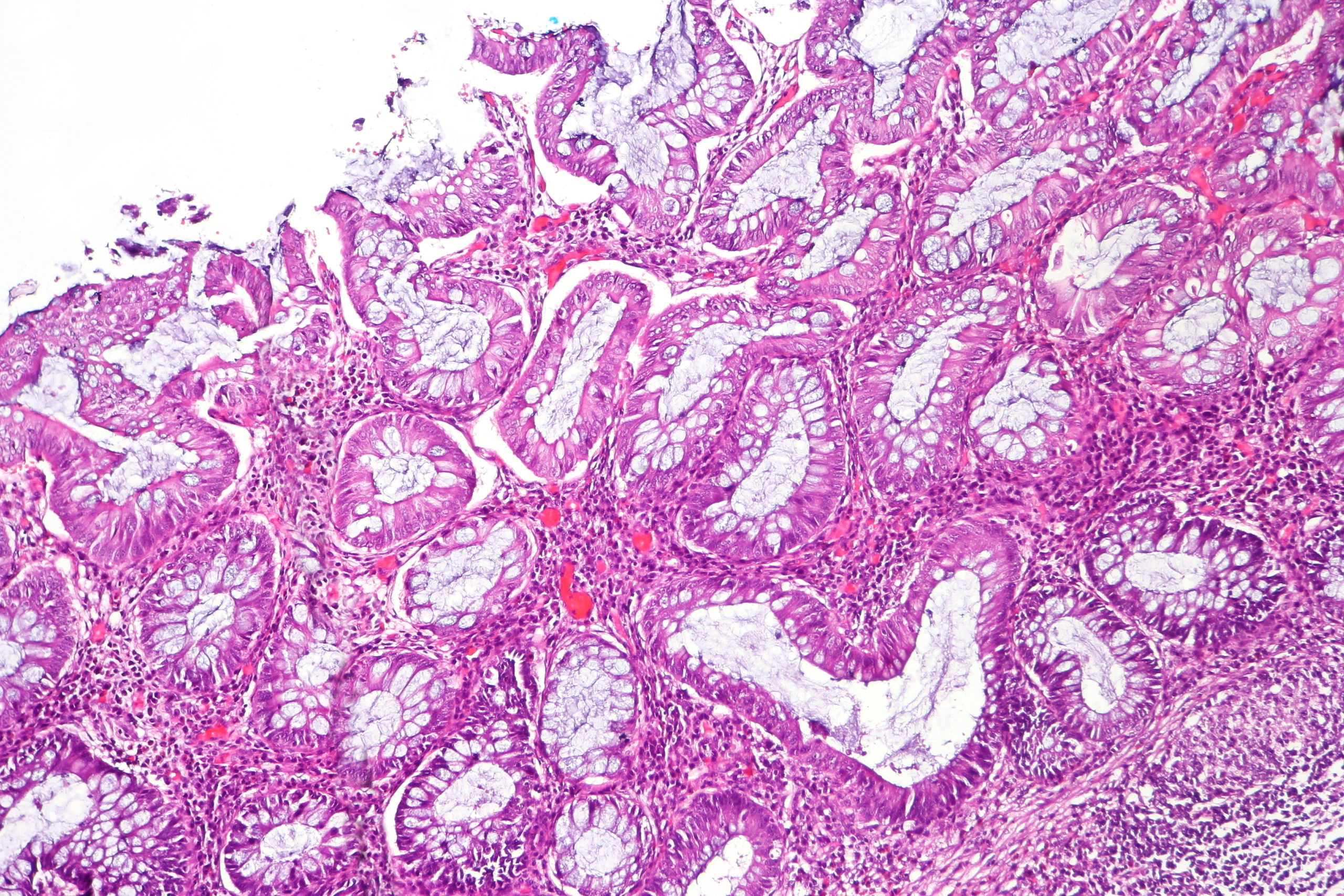
Eliquis has contraindications like active pathological bleeding and severe hypersensitivity reactions. Recognize these contraindications and stop Eliquis immediately during active pathological hemorrhage. Eliquis elevates bleeding risk, possibly causing severe or fatal bleeding. Report any signs of blood loss promptly and seek medical help.
| Considerations | Recommendations |
|---|---|
| Premature discontinuation of Eliquis | Continue taking Eliquis as prescribed, unless for pathological bleeding or upon completing the therapy |
| Neuraxial anesthesia or spinal puncture | Weigh the risks and benefits carefully for patients on Eliquis |
| Active pathological bleeding | Promptly discontinue Eliquis |
| Signs or symptoms of bleeding | Report immediately and seek medical attention |
Overall, it is crucial to adhere to the safety considerations for Eliquis to ensure the most effective and safe use of the medication. Regular monitoring, prompt reporting of any bleeding or symptoms, and close communication with your healthcare professional are essential for managing the potential risks associated with Eliquis.
Efficacy of Eliquis in Preventing Stroke and Systemic Embolism
Eliquis has been proven to be highly effective in reducing the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation (NVAF). Clinical trials have shown that Eliquis is superior to the older anticoagulant warfarin in preventing these dangerous events.
In a study comparing Eliquis to warfarin, Eliquis significantly reduced the incidence of stroke and systemic embolism compared to placebo. This highlights the powerful impact that Eliquis can have in improving patient outcomes and reducing the risk of life-threatening complications.
Patients with NVAF who are at higher risk for stroke and systemic embolism are recommended to take Eliquis as part of their treatment plan. It is important to note, however, that the risk of bleeding should always be considered when using any anticoagulant therapy.
Eliquis vs. Warfarin in Stroke Prevention
| Eliquis | Warfarin | |
|---|---|---|
| Effectiveness in reducing stroke and systemic embolism | Highly effective | Less effective compared to Eliquis |
| Regular monitoring required | Less frequent monitoring | Frequent monitoring of International Normalized Ratio (INR) levels |
| Drug interactions | Fewer drug interactions | Potential for multiple drug interactions |
| Dietary restrictions | No dietary restrictions | Requires careful management of vitamin K intake |
Note: The table above compares the efficacy and monitoring requirements of Eliquis and warfarin in stroke prevention. It is important to consult with a healthcare professional to determine the most appropriate anticoagulant therapy based on individual patient characteristics and medical history.
By choosing Eliquis as part of a comprehensive treatment plan, patients with NVAF can significantly reduce their risk of stroke and systemic embolism. It is crucial to closely follow the guidance of healthcare professionals and adhere to the prescribed dosage to maximize the benefits of Eliquis.
Blood Clot Prevention Tips
Alongside medical treatment like Eliquis, there are several measures you can take to naturally prevent blood clots. Incorporating these tips into your daily routine can help reduce your risk and promote overall cardiovascular health.
Lifestyle Modifications
- Maintain a healthy weight: Obesity increases the risk of blood clots, so aim for a healthy body weight through a balanced diet and regular exercise.
- Exercise regularly: Engage in physical activity such as walking, jogging, or swimming to improve blood circulation and reduce the likelihood of clot formation.
- Avoid prolonged periods of sitting: Take breaks every hour to stand up, stretch, and move around, especially if you have a sedentary job.
- Stay hydrated: Proper hydration helps prevent your blood from becoming too thick, reducing the risk of clotting. Drink plenty of water throughout the day.
By incorporating these lifestyle modifications, you can significantly reduce your risk of blood clots and support your overall well-being.
Healthy Habits
- Avoid smoking: Smoking damages blood vessels and promotes clot formation. Quitting smoking significantly reduces your risk of developing blood clots.
- Control blood pressure: High blood pressure can damage blood vessels and increase the risk of clot formation. Monitor your blood pressure regularly and follow your healthcare professional’s recommendations for management.
- Manage cholesterol levels: High cholesterol can contribute to the formation of plaque in blood vessels, increasing the risk of clotting. Maintain a healthy diet and talk to your healthcare professional about managing your cholesterol levels.
These healthy habits can have a positive impact on your cardiovascular health and help minimize the risk of blood clots.
Medical Considerations
If you have a medical condition that increases your risk of blood clots, consult with your healthcare professional for personalized advice and preventive measures. They may recommend additional strategies such as the use of compression stockings or medication to further reduce your risk.
It is important to speak with a healthcare professional to determine the best approach to blood clot prevention based on individual risk factors and medical history.
Comparing Eliquis to Other Oral Anticoagulants
Eliquis, a factor Xa inhibitor, offers advantages over warfarin in preventing blood clots due to its targeted action. As a direct oral anticoagulant (DOAC), Eliquis, unlike dabigatran, has broader applications, including NVAF stroke prevention, DVT prophylaxis, and treatment of DVT and PE. Understanding Eliquis’ mechanism compared to other anticoagulants highlights its unique benefits.
| Medication | Mechanism of Action |
|---|---|
| Eliquis (Apixaban) | Factor Xa inhibitor |
| Warfarin | Vitamin K antagonist |
| Dabigatran | Direct thrombin inhibitor |
As shown in the table above, Eliquis targets factor Xa, while warfarin inhibits vitamin K, and dabigatran directly inhibits thrombin. Each medication has a different target in the clotting cascade, resulting in variations in their efficacy, required monitoring, and potential side effects.
Ultimately, the choice between different oral anticoagulants should be individualized based on patient characteristics, such as renal function, hepatic function, and concomitant medications. Your healthcare professional can guide you in selecting the most suitable anticoagulant based on your specific needs and medical history.
Eliquis for Non-Insured Patients
For patients who are not insured or have limited insurance coverage, the cost of Eliquis may be a concern. However, there are options available to help reduce the cost and make it more affordable. Patient assistance programs offered by pharmaceutical companies can provide financial assistance to eligible individuals. These programs can help cover the cost of medication, including Eliquis, for qualifying patients. It is recommended to check with the manufacturer or your healthcare provider to explore these programs and determine if you are eligible.
In addition to patient assistance programs, another option is to consider purchasing Eliquis online from reputable online pharmacies.
Buying medications online can sometimes offer discounted prices compared to traditional brick-and-mortar pharmacies. However, it is important to exercise caution and ensure that the online pharmacy is legitimate and operates within the legal framework for prescription medications. Look for pharmacies that require a valid prescription and have a secure payment system to protect your personal information.
When considering purchasing Eliquis online, be sure to compare prices from different online pharmacies to ensure you are getting the best deal. It is also recommended to consult with your healthcare provider or pharmacist before making any changes to your medication or buying it from an online source. They can provide guidance and help ensure that you are receiving genuine medication that is safe and effective for your specific needs.
| Option | Pros | Cons |
|---|---|---|
| Patient Assistance Programs | – Financial assistance for eligible patients – Covers the cost of medication – Provided directly by pharmaceutical companies |
– Eligibility requirements – May have limited availability – Requires application process |
| Online Pharmacies | – Potentially lower prices – Convenient and accessible – Wide range of options |
– Risk of counterfeit or substandard medication – Legal and safety concerns – Lack of face-to-face interaction with healthcare professionals |
Conclusion
For non-insured patients, accessing affordable medication like Eliquis can be challenging. However, patient assistance programs and online pharmacies can offer potential solutions to help reduce the cost of Eliquis and make it more accessible. It is important to evaluate these options carefully, ensuring their legitimacy and adherence to legal and safety standards. Consulting with healthcare professionals and healthcare providers is essential to make informed decisions and prioritize patient safety and well-being.
Know the potential risks and side effects of Eliquis when you use it. Eliquis can cause bleeding, ranging from mild to severe or even fatal. Watch for signs like frequent nosebleeds, unexplained bruises, or blood in urine or stool, and seek immediate medical help if you notice any.
Additionally, Eliquis may elevate liver enzymes, indicating liver issues. Get regular blood tests to check liver function while on this medication. Tell your doctor about all medications, including over-the-counter drugs and supplements, as they might increase bleeding risk when combined with Eliquis.
Remember, Eliquis is an anticoagulant. Using it with other anticoagulants or antiplatelet drugs can heighten bleeding risk. Always follow your doctor’s guidance on other medications when taking Eliquis. Be cautious of potential drug interactions and consult your doctor before starting any new medication or supplement.
In conclusion, Eliquis effectively prevents blood clots and lowers stroke risk. However, stay vigilant about its potential risks and side effects. Regular check-ups, recognizing bleeding symptoms, and discussing all your medications with your doctor are vital for your safety while using Eliquis.
| Adverse Reactions | Bleeding Risk | Anticoagulants and Antiplatelet Agents |
|---|---|---|
| – Elevated liver transaminases | – Risk of bleeding, ranging from mild to severe | – Eliquis should not be combined with other anticoagulants without healthcare provider approval |
| – Potential drug interactions | – Symptoms of bleeding include frequent nosebleeds, unexplained bruising, and blood in urine or stool | – Combining Eliquis with antiplatelet agents can further increase the risk of bleeding |
| – Regular monitoring of liver function recommended | – Immediate medical attention is necessary if bleeding symptoms occur | – Consult healthcare provider before starting any new medications or supplements |
The Importance of Regular Monitoring and Follow-up
Monitoring patients on Eliquis is essential for treatment safety and efficacy. Regular healthcare check-ups help manage anticoagulant therapy. During these visits, professionals assess adherence, monitor bleeding signs, and address patient concerns.
Vigilance for neurological impairment signs is crucial. Rarely, Eliquis patients may develop spinal or epidural hematomas from procedures like spinal puncture. Immediate medical attention for any neurological symptoms is vital to prevent long-term paralysis.
Regular check-ups also help evaluate Eliquis therapy response. Professionals can assess bleeding risk, medication effectiveness, and adjust treatment as needed. This ensures patients receive optimal Eliquis dosage and duration for their condition.
Summary:
Regularly monitor Eliquis patients to assess therapy adherence, detect signs of bleeding, and address concerns. Evaluate Eliquis effectiveness in preventing clots and reducing stroke risk. Educate patients on recognizing neurological impairment symptoms and prompt medical attention.
The Role of Eliquis in Preventing Blood Clots and Reducing Stroke Risk
Eliquis, or apixaban, prevents blood clots and stroke in nonvalvular atrial fibrillation (NVAF) patients. It inhibits factor Xa, reducing thrombin generation and clot formation. Yet, Eliquis carries risks, including increased bleeding risk.
Monitoring Eliquis patients is essential for correct usage and treatment safety. Regular healthcare visits help detect bleeding signs and ensure therapy adherence.
Besides medication, lifestyle changes can naturally prevent blood clots. Maintaining a healthy weight, controlling blood pressure, and cholesterol through exercise can lower clot and stroke risks.
Combining Eliquis benefits with lifestyle changes reduces clot and stroke risks. Always consult your healthcare professional for personalized advice based on your medical history and risk factors.
FAQ
What is Eliquis used for?
Eliquis is used to lower the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation (NVAF).
How does Eliquis work?
Eliquis inhibits the clotting protein factor Xa, reducing the formation of blood clots.
When should Eliquis be discontinued?
Patients should only discontinue Eliquis for pathological bleeding or upon completion of a prescribed course of therapy.
What are the potential risks of Eliquis?
Premature discontinuation of Eliquis increases the risk of thrombotic events, and it may cause spinal or epidural hematomas in patients undergoing certain procedures.
Are there any natural ways to prevent blood clots?
Yes, maintaining a healthy lifestyle, regular exercise, avoiding prolonged periods of immobility, and staying hydrated can help prevent blood clots.
How does Eliquis compare to warfarin?
Eliquis offers advantages over warfarin, including a more predictable anticoagulant effect and fewer drug interactions.
What options are available to reduce the cost of Eliquis?
Patient assistance programs offered by pharmaceutical companies and discounts through online pharmacies may help reduce the cost of Eliquis.
What are the potential side effects of Eliquis?
The most common side effects are related to bleeding, and elevated liver transaminases can also occur. Patients should be educated about the signs and symptoms of bleeding and seek immediate medical attention if they occur.
How often should patients receiving Eliquis be monitored?
Patients should be regularly monitored by their healthcare professional for signs of bleeding and adherence to therapy.
What is the role of Eliquis in preventing blood clots and reducing stroke risk?
Eliquis plays a crucial role in preventing blood clots and reducing the risk of stroke, particularly in patients with nonvalvular atrial fibrillation.
Source Links
- https://www.eliquis.com/eliquis/hcp
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3684191/
- https://news.bms.com/news/details/2023/Retrospective-Observational-Study-Assessing-Real-World-Clinical-Impact-of-Switching-or-Continuing-Eliquis-or-Rivaroxaban-Presented-at-the-European-Society-of-Cardiology-ESC-Congress-2023/default.aspx