Psoriatic arthritis (PsA) is a chronic, inflammatory disease that affects the joints and entheses, often appearing between the ages of 30 and 50. It can cause significant joint damage if left untreated and is associated with related health conditions.
Stelara is a medication used to treat moderately to severely active PsA in both adults and children aged 6 and older. Working closely with a rheumatologist is crucial to finding the right treatment plan for PsA.
Key Takeaways:
- Psoriatic arthritis is a chronic, inflammatory disease that affects the joints and entheses.
- Stelara is a medication used to treat moderately to severely active PsA in adults and children aged 6 and older.
- Early recognition, diagnosis, and treatment of PsA are important to prevent extensive joint damage.
- Working with a rheumatologist is essential in determining the most suitable treatment plan for PsA.
- Stelara works by targeting specific proteins in the immune system to reduce inflammation in the joints.
Understanding Psoriatic Arthritis
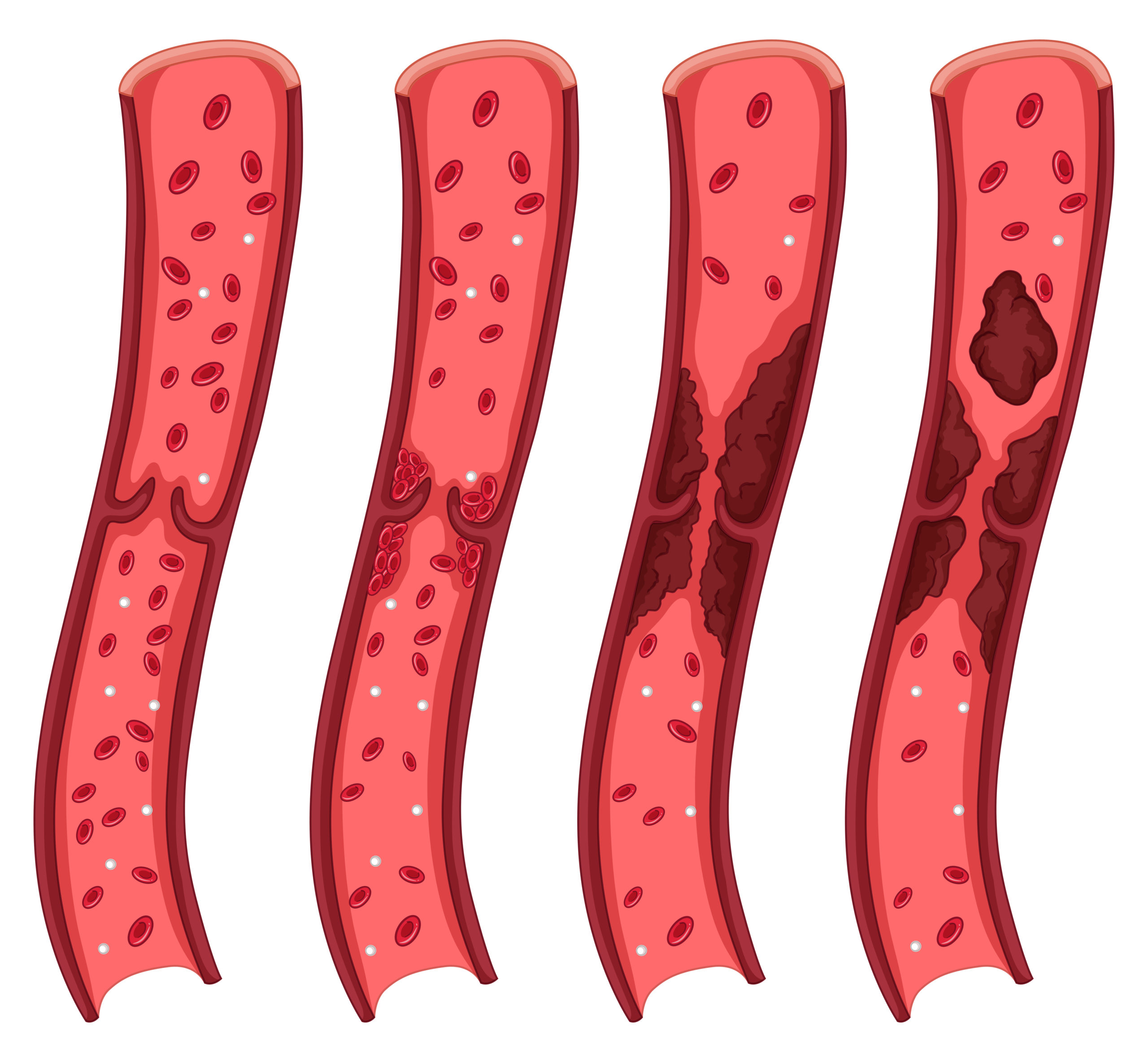
Psoriatic arthritis is a chronic, inflammatory disease that affects both the joints and the entheses, which are the areas where tendons and ligaments connect to bone. This condition is closely associated with psoriasis, a skin condition characterized by red, scaly patches. Psoriatic arthritis can develop at any age, although it often appears about 10 years after psoriasis first presents itself. If left untreated, psoriatic arthritis can lead to extensive joint damage, making early recognition, diagnosis, and treatment crucial for managing the disease.
When it comes to understanding psoriatic arthritis, it is essential to work closely with a rheumatologist. These specialized doctors have expertise in diagnosing and treating immune system-related joint, bone, and muscle conditions. They can help assess the severity of the disease and develop a comprehensive treatment plan tailored to each individual’s needs.
Key points to understand about psoriatic arthritis:
- It is a chronic, inflammatory disease that affects the joints and entheses.
- It is commonly associated with psoriasis.
- Early recognition, diagnosis, and treatment are crucial to prevent extensive joint damage.
- Rheumatologists specialize in diagnosing and treating immune system-related joint conditions.
“Psoriatic arthritis is more than a joint problem; it is a systemic condition that requires comprehensive management. Working with a rheumatologist is essential for accurate diagnosis, appropriate treatment, and ongoing monitoring of the disease.”
A rheumatologist can provide a range of treatment options, including medications like Stelara. These medications target the underlying inflammation, reducing symptoms and preventing further joint damage. Through regular follow-up visits, a rheumatologist can monitor the progress of the disease and adjust the treatment plan accordingly, ensuring optimal management of psoriatic arthritis.
| Treatments |
Description |
| Medications |
Including Stelara, medications can help reduce inflammation and manage symptoms. |
| Physical therapy |
Exercises and techniques to improve joint function and reduce pain. |
| Lifestyle modifications |
Including maintaining a healthy weight, regular exercise, and stress management. |
Understanding psoriatic arthritis means recognizing its impact on joints and entheses, linking it with psoriasis, and prioritizing early diagnosis and treatment. Collaborate with a rheumatologist to manage the disease effectively and create a personalized treatment plan that may involve medications like Stelara. By tackling the root inflammation and adopting a holistic approach, people with psoriatic arthritis can live a more comfortable and active life.
Available Treatments for Psoriatic Arthritis
Psoriatic arthritis demands a thorough treatment plan to effectively manage its symptoms. While no cure exists, various treatments can slow disease progression, ease pain, safeguard joints, and preserve mobility.
This medication stands as a viable treatment for psoriatic arthritis. Approved for adults and children aged 6 and up with active psoriatic arthritis, this medication targets specific immune system proteins that fuel inflammation. This action helps diminish joint inflammation and relieve symptoms
Treatment Options for Psoriatic Arthritis:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications can help reduce pain and inflammation.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs can help slow down disease progression and protect joints.
- Biologic therapies: Biologic therapies like Stelara target specific proteins in the immune system to reduce inflammation in the joints.
- Corticosteroids: Corticosteroids may be used to reduce inflammation and manage severe symptoms.
It is important to consult with a healthcare professional, such as a rheumatologist, to determine the most suitable treatment plan for psoriatic arthritis. The choice of treatment will depend on factors such as the severity of the disease, the individual’s response to previous therapies, and any other related health conditions they may have.
| Treatment Option |
Description |
Pros |
Cons |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) |
Medications that help reduce pain and inflammation. |
– Effective in managing mild to moderate pain.
– Available over-the-counter or by prescription. |
– May cause gastrointestinal side effects.
– Not suitable for long-term use. |
| Disease-modifying antirheumatic drugs (DMARDs) |
Medications that slow down disease progression and protect joints. |
– Can help prevent joint damage.
– May improve overall quality of life. |
– May take time to show noticeable effects.
– Potential side effects. |
| Biologic therapies (e.g., Stelara) |
Medications that target specific proteins in the immune system to reduce inflammation in the joints. |
– Highly effective in reducing symptoms.
– Can help slow down disease progression. |
– Costly treatment option.
– Requires regular injections. |
| Corticosteroids |
Medications that reduce inflammation and manage severe symptoms. |
– Provides quick relief from inflammation.
– Can be administered orally, topically, or through injections. |
– Potential for long-term side effects.
– Not suitable for long-term use. |
With the range of treatment options available, individuals with psoriatic arthritis can work closely with their healthcare professionals to find the most suitable approach for managing their condition. It is important to discuss the potential benefits and risks of each treatment option to make an informed decision and optimize the management of psoriatic arthritis.
The Role of Stelara in Psoriatic Arthritis Treatment
This treatment aids Psoriatic Arthritis (PsA) by targeting immune system proteins causing inflammation. By blocking these proteins, it reduces joint inflammation and eases symptoms.
The mechanism of action involves inhibiting interleukin-12 (IL-12) and interleukin-23 (IL-23), key cytokines in inflammation and immune response. Suppressing these cytokines alleviates PsA symptoms like joint pain and swelling.
Administered via injections, this treatment can be given at a healthcare office or self-administered at home. Adhering to prescribed dosages and instructions is crucial.
Benefits of Slelara in Psoriatic Arthritis Treatment
This treatment offers notable benefits for PsA patients. By addressing inflammation, it relieves joint pain, stiffness, and swelling, enhancing joint comfort and mobility. A study stated, “It significantly improves joint comfort and reduces skin inflammation.”
Beyond joint relief, this treatment enhances skin health in PsA patients with psoriasis, reducing its severity and occurrence.
In conclusion, this treatment is pivotal in PsA management. It targets inflammation, alleviates symptoms, and enhances joint comfort and skin health, promoting an active, fulfilling life.
| Benefits of Stelara in Psoriatic Arthritis Treatment |
| Reduces joint pain, stiffness, and swelling |
| Improves overall joint comfort |
| Reduces skin inflammation in individuals with psoriasis |
| Allows individuals to lead a more fulfilling and active life |
| Minimizes the impact of PsA on daily activities |
Ensuring Efficacy and Safety of Stelara
Stelara has been extensively studied in clinical trials to establish its effectiveness and safety in treating Psoriatic Arthritis (PsA). These trials have shown that Stelara is an effective medication for managing the symptoms of PsA and reducing inflammation in the joints. It works by targeting specific proteins in the immune system that contribute to inflammation, providing relief from joint pain and stiffness.
While Stelara has shown significant benefits in treating PsA, it is important to be aware of potential side effects. Common side effects of Stelara may include upper respiratory infections, injection site reactions, headache, and fatigue. It is crucial to discuss these potential side effects with a healthcare professional and weigh the benefits against the risks before starting treatment with Stelara.
“Stelara has been proven to be highly effective in managing the symptoms of Psoriatic Arthritis. It has helped many patients experience relief from joint pain and improved overall quality of life.”
To ensure the safety and efficacy of Stelara treatment, it is essential to follow the prescribed dosage and administration instructions provided by your healthcare professional. Regular follow-up visits with your rheumatologist are important to monitor your progress and make any necessary adjustments to your treatment plan. Your healthcare professional will work closely with you to assess the severity of your PsA and determine the most suitable treatment approach.
| Benefits of Stelara Treatment for Psoriatic Arthritis |
Potential Side Effects of Stelara |
| Reduced joint pain and stiffness |
Upper respiratory infections |
| Improved overall quality of life |
Injection site reactions |
| Decreased inflammation in the joints |
Headache |
| Relief from PsA symptoms |
Fatigue |
When considering Stelara as a treatment option for PsA, it is important to have an open and honest discussion with your healthcare professional. They will be able to provide you with the necessary information about the benefits, potential side effects, and overall safety of Stelara. Together, you can make an informed decision about whether Stelara is the right choice for your Psoriatic Arthritis treatment.
Managing Psoriatic Arthritis Symptoms
Managing psoriatic arthritis (PsA) symptoms effectively improves life quality. Besides medication, lifestyle changes significantly reduce pain and inflammation. Consider these active strategies:
- Engage in regular exercise: Low-impact activities like swimming, yoga, or walking enhance joint mobility and reduce stiffness. Consult a healthcare professional for the best exercise plan.
- Keep a healthy weight: Excess weight strains joints, aggravating PsA symptoms. Balanced diet and exercise help maintain a healthy weight, easing joint pressure.
- Use joint protection techniques: Supportive devices like braces or splints relieve joint pain. Avoid strenuous activities to prevent flare-ups.
- Apply hot and cold therapy: Use heat or cold packs on affected joints to reduce inflammation and get temporary pain relief. Experiment to find the most effective method.
- Manage stress: Stress exacerbates PsA symptoms. Practice relaxation techniques like deep breathing, meditation, or engage in enjoyable activities to reduce stress and boost well-being.
Though these strategies aid PsA symptom management, collaborating with a healthcare professional for a comprehensive treatment plan is crucial. They may suggest a treatment like Stelara to reduce inflammation and prevent symptom flare-ups. Stelara targets specific immune system proteins, offering relief from joint and skin PsA symptoms.
Keep in mind, PsA experiences vary. Find a tailored treatment plan through lifestyle changes and healthcare guidance to effectively manage symptoms and lead a satisfying life.
| Lifestyle Modifications |
Benefits |
| Regular exercise |
Improves joint mobility and reduces stiffness |
| Maintaining a healthy weight |
Relieves pressure on joints |
| Joint protection techniques |
Provides support and alleviates pain |
| Hot and cold therapy |
Reduces inflammation and provides pain relief |
| Stress management |
Reduces stress and improves overall well-being |
Working with a Rheumatologist
When it comes to managing your Psoriatic Arthritis (PsA), collaborating with a rheumatologist is crucial. These specialized healthcare professionals have expertise in diagnosing and treating immune system-related joint, bone, and muscle conditions. By working with a rheumatologist, you can ensure that you receive the most comprehensive treatment plan tailored to your specific needs.
A rheumatologist will assess the severity of your PsA and develop a personalized treatment plan that may include medications like Stelara. They will closely monitor your progress over time, making adjustments to the treatment plan as necessary to achieve optimal management of your PsA symptoms.
Regular follow-up visits with a rheumatologist are essential to track your response to treatment, address any concerns or side effects, and make any necessary changes to your medication or therapy. By maintaining a strong partnership with your rheumatologist, you can stay informed and actively participate in your PsA treatment journey.
Why Work with a Rheumatologist?
Rheumatologists specialize in the diagnosis and treatment of autoimmune and inflammatory conditions, including PsA. Their in-depth knowledge and experience enable them to accurately diagnose your condition, determine the appropriate treatment options, and provide ongoing guidance and support throughout your PsA journey.
A rheumatologist will help you develop a tailored treatment plan that may include Stelara and other interventions to effectively manage your PsA symptoms. They will also closely monitor your progress, assessing the efficacy of the treatment and making any necessary adjustments to optimize outcomes.
The Importance of a Personalized Treatment Plan
PsA is a highly individualized condition, and each person may respond differently to various treatments. A rheumatologist will work closely with you to understand your unique symptoms, medical history, and lifestyle factors. This information allows them to create a personalized treatment plan that considers your specific needs and preferences.
Your rheumatologist will assess treatment options like Stelara, discussing benefits, risks, and alternatives. Collaborating ensures confident PsA treatment decisions and access to latest advancements.
| Rheumatologist Benefits |
| Specialized expertise in immune system-related joint conditions |
| Accurate diagnosis of PsA |
| Personalized treatment plan tailored to your specific needs |
| Close monitoring of treatment progress and adjustments as needed |
| Access to the latest advancements in PsA treatment |
Benefits of Stelara Treatment
Stelara offers significant benefits for individuals with Psoriatic Arthritis (PsA), providing relief from joint discomfort and improving skin health. By targeting inflammation in the immune system, Stelara helps reduce pain, alleviate joint stiffness, and enhance overall quality of life. With its proven mechanism of action, Stelara addresses both joint and skin symptoms associated with PsA, offering comprehensive relief.
Studies have shown that Stelara effectively improves joint comfort, allowing individuals to engage in daily activities with greater ease. By reducing inflammation, Stelara can minimize symptom flare-ups and provide lasting relief for PsA patients. Additionally, improved skin health is another key benefit of Stelara treatment. The medication’s targeted approach to inflammation helps reduce the skin inflammation commonly associated with PsA, leading to healthier and clearer skin.
By incorporating Stelara into a personalized treatment plan, individuals with PsA can experience a significant improvement in their overall well-being. Working closely with a rheumatologist, patients can address their specific needs and customize their treatment approach to maximize the benefits of Stelara. Whether it’s relieving joint discomfort or enhancing skin health, Stelara offers a comprehensive solution to manage the symptoms of PsA and improve daily life.
Finding the Right Treatment Plan
When it comes to managing psoriatic arthritis (PsA), finding the right treatment plan is crucial. Every individual’s PsA may vary in terms of severity and response to treatment. That’s why it’s important to collaborate with a healthcare professional who specializes in immune system-related joint, bone, and muscle conditions, such as a rheumatologist.
A rheumatologist can assess the severity of your PsA and recommend appropriate interventions, including medications like Stelara. Together, you can develop a personalized treatment plan that takes into account your specific needs and goals. It’s essential to have open and honest communication with your healthcare professional to ensure the best possible outcomes.
Stelara is one of the treatment options available for PsA. However, it’s essential to discuss the potential benefits, risks, and alternatives with your rheumatologist to make an informed decision. They will consider factors such as your medical history, overall health, and response to previous treatments to determine if Stelara is the right choice for you.
Accessing Stelara for Psoriatic Arthritis Treatment
If you or a loved one has been diagnosed with Psoriatic Arthritis (PsA), accessing the right treatment is essential for managing the condition effectively. Stelara is a medication that has shown significant benefits in alleviating the symptoms of PsA, including joint discomfort and skin inflammation. However, it is important to understand how to access Stelara for your PsA treatment needs.
First and foremost, Stelara is a prescription medication, which means it can only be obtained through a healthcare professional. It is crucial to consult with a rheumatologist, who specializes in treating immune system-related joint, bone, and muscle conditions like PsA. Your rheumatologist will evaluate your condition and determine if Stelara is a suitable treatment option for you.
For those who are uninsured or facing financial challenges, there are options available to help make Stelara more affordable. Prescription assistance programs and insurance coverage may be accessible, providing support in obtaining the medication you need for your PsA treatment. It is recommended to discuss these options with your healthcare professional to explore the possibilities and ensure access to necessary psoriatic arthritis treatment.
Remember, Stelara is just one option among many for treating PsA. By working closely with a rheumatologist and discussing your specific needs and preferences, you can determine the most suitable treatment plan to manage your PsA effectively and improve your joint comfort and skin health.
Leading a Life of Joint Comfort and Improved Skin Health
Living with psoriatic arthritis (PsA) can be challenging, but with the right treatment, such as Stelara, you can experience improved joint comfort and skin health. By working closely with a rheumatologist and following a personalized treatment plan, you can manage the symptoms and regain control of your life.
PsA can cause joint pain, stiffness, swelling, and skin changes, which can significantly impact your daily activities. Stelara, a medication specifically designed for PsA, targets the underlying inflammation and helps reduce these symptoms. By alleviating pain, reducing joint stiffness, and improving overall skin health, Stelara can enhance your quality of life.
Your rheumatologist will develop a comprehensive treatment plan tailored to your specific needs. This plan may include Stelara, along with other interventions such as exercise, weight management, and joint protection techniques. Regular follow-up visits with your rheumatologist are crucial to monitor your progress and make any necessary adjustments to your treatment plan.
Remember, with proper care and support, the burden of PsA can be minimized. By taking proactive steps to manage your condition and utilizing the benefits of Stelara, you can lead a fulfilling and active life, enjoying joint comfort and improved skin health.
FAQ
What is Psoriatic Arthritis?
Psoriatic arthritis is a chronic, inflammatory disease that affects the joints and entheses, where tendons and ligaments connect to bone. It is often associated with psoriasis and related health conditions.
When does Psoriatic Arthritis typically appear?
Psoriatic arthritis often appears between ages 30 and 50, but it can start at any age and may appear about 10 years after psoriasis develops.
What can happen if Psoriatic Arthritis is left untreated?
If left untreated, Psoriatic Arthritis can cause extensive joint damage.
What is Stelara?
Stelara is a medication used to treat moderately to severely active Psoriatic Arthritis in adults and children ages 6 and older.
How does Stelara work?
Stelara works by targeting specific proteins in the immune system that contribute to inflammation, helping to reduce inflammation in the joints and alleviate the symptoms of Psoriatic Arthritis.
What are the common side effects of Stelara?
Common side effects of Stelara may include upper respiratory infections, injection site reactions, headache, and fatigue.
What lifestyle modifications can help manage Psoriatic Arthritis symptoms?
Regular exercise, maintaining a healthy weight, and applying proper joint protection techniques can help reduce pain and improve joint function.
Why is it important to work with a rheumatologist for Psoriatic Arthritis?
Rheumatologists specialize in diagnosing and treating immune system-related joint, bone, and muscle conditions, including Psoriatic Arthritis.
How can Stelara benefit individuals with Psoriatic Arthritis?
Stelara can provide relief by reducing inflammation, minimizing symptom flare-ups, and improving joint comfort and skin health.
How can I access Stelara for Psoriatic Arthritis treatment?
Stelara is a prescription medication that should be obtained through a healthcare professional. Prescription assistance programs and insurance coverage may be available to make it more affordable.
Can Psoriatic Arthritis be managed effectively?
With the right treatment plan, such as Stelara, Psoriatic Arthritis can be managed effectively, allowing individuals to lead a fulfilling and active life.
Source Links